- Home
- Antibiotic Awareness Week 2021 Outpatient Parenteral Antimicrobial Stewardship
Outpatient Parenteral Antimicrobial Stewardship |
Briefly describe your daily role as an antimicrobial stewardship pharmacistMy primary responsibilities are rounding with the inpatient ID consult team and performing daily prospective audit and feedback on selected antimicrobials. I target patients who are on broad spectrum, restricted, and/or duplicative antimicrobial therapy. I also review patients with positive blood cultures daily. I make every effort to convey recommendations and education to medical teams in person as frequently as possible. I collaborate with our critical care, internal medicine, and staff pharmacists closely when communicating recommendations to the primary teams. Throughout the day I also answer questions from medical providers, pharmacists, nurses, case managers, home health home infusion companies, and patients. Our pharmacy team is heavily involved in the discharge process. I work with our case managers and authorization specialists to ensure antimicrobials are covered, and I provide input on placement for IV antibiotics to facilitate discharges. Once a week, I see patients on long-term IV antibiotics at the Outpatient Parenteral Antimicrobial Therapy (OPAT) clinic through a combination of telephone and in-person visits. The remainder of my time is spent performing medication use evaluations, implementing quality improvement projects, attending various department meetings to promote antimicrobial stewardship, leading the antimicrobial stewardship committee, and precepting pharmacy residents and students. During the COVID-19 pandemic, a great deal of my time is also spent on keeping up-to-date on therapeutics and creating medication use criteria.What OPAT stewardship initiative or antibiotic awareness effort are you most proud of that you have participated in or led?Effective communication is essential to safe care transitions. This is especially true for patients being discharged on IV antibiotics or OPAT. An accurate and complete OPAT order not only consists of the right antibiotic, dosing instructions, and duration of therapy, but also information about vascular access maintenance care such as normal saline or heparin flushes, vascular access dressing changes, whether vascular access should be maintained or discontinued after the end of therapy, the name and contact information of the managing providers, and appropriate laboratory monitoring parameters. At our institution, I led the initiative in creating an OPAT orderset that contains these necessary components based on the types of antimicrobials and vascular access present. Prior to the OPAT orderset, our medical residents had to free type these order details on a blank electronic prescription box! You can imagine the enormous room for errors and mistakes. It is difficult to remember all the details that go into creating a complete OPAT order. Often times weekly laboratory monitoring orders and vascular access maintenance orders were missing. In addition to being a medication safety issue, it also created many unnecessary phone calls and frustration between home health companies, home infusion pharmacies, the primary team, and case managers. Creating the orderset was a collaborative effort; I involved leadership from various disciplines including medical residents, attendings, case managers, home health companies, home infusion pharmacies, and IT. After implementing the orderset, all OPAT orders at discharge contains all necessary components and it greatly improved efficacy and satisfaction of our medical residents and case managers!What does "Being Antibiotics Aware" mean to you?Unlike other medications, antibiotics are shared resources. How we use antibiotics today affects their effectiveness in the future. Being antibiotic aware means promoting a culture of judicious use of antibiotics – doing our best to balance using antibiotics to treat the patient in front of us and re-evaluating the needs for antibiotics to minimize unintended consequences. One of the biggest rewards of being an antimicrobial stewardship pharmacist is seeing providers streamline or discontinue antibiotics on their own without prompting! Antibiotic stewardship is not a one-person job; it’s a team effort and we need all prescribers to engage and be antibiotic aware.What is one pearl you have for all pharmacists to help them be antibiotic stewards?Approach antibiotic stewardship from a therapy and care optimization perspective. Antibiotic stewardship is not always about de-escalating or discontinuing antibiotics, rather it is about collaborating with providers to optimize antimicrobial therapies for patients. For example, it is never too early to think about discharge planning. If a patient is on IV antibiotic for bacterial infection in the hospital, we can start assessing options for oral antibiotics and duration of therapy once patient is clinically stable and a final diagnosis has been made. Communicate the recommendation with the team as soon as the patient is stable. If IV antibiotic is desired for discharge, consider recommending the case to be reviewed by the infectious diseases or antimicrobial stewardship team. Doing the right thing for the patient will eventually leads to improved patient outcome and avoidance of patients being re-admitted to the hospital for the same infection. The CDC has great resource on how all healthcare professionals can be antibiotic aware at hospital discharge!https://www.cdc.gov/antibiotic-use/pdfs/BAA-Hospital-Discharge-Flowchart-P.pdf Acknowledgement: The Kern Medical OPAT program would not be possible without the support from the Infectious Diseases team and Dr. Rasha Kuran. | Isabel Fong, PharmD, BCIDP, AAHIVP
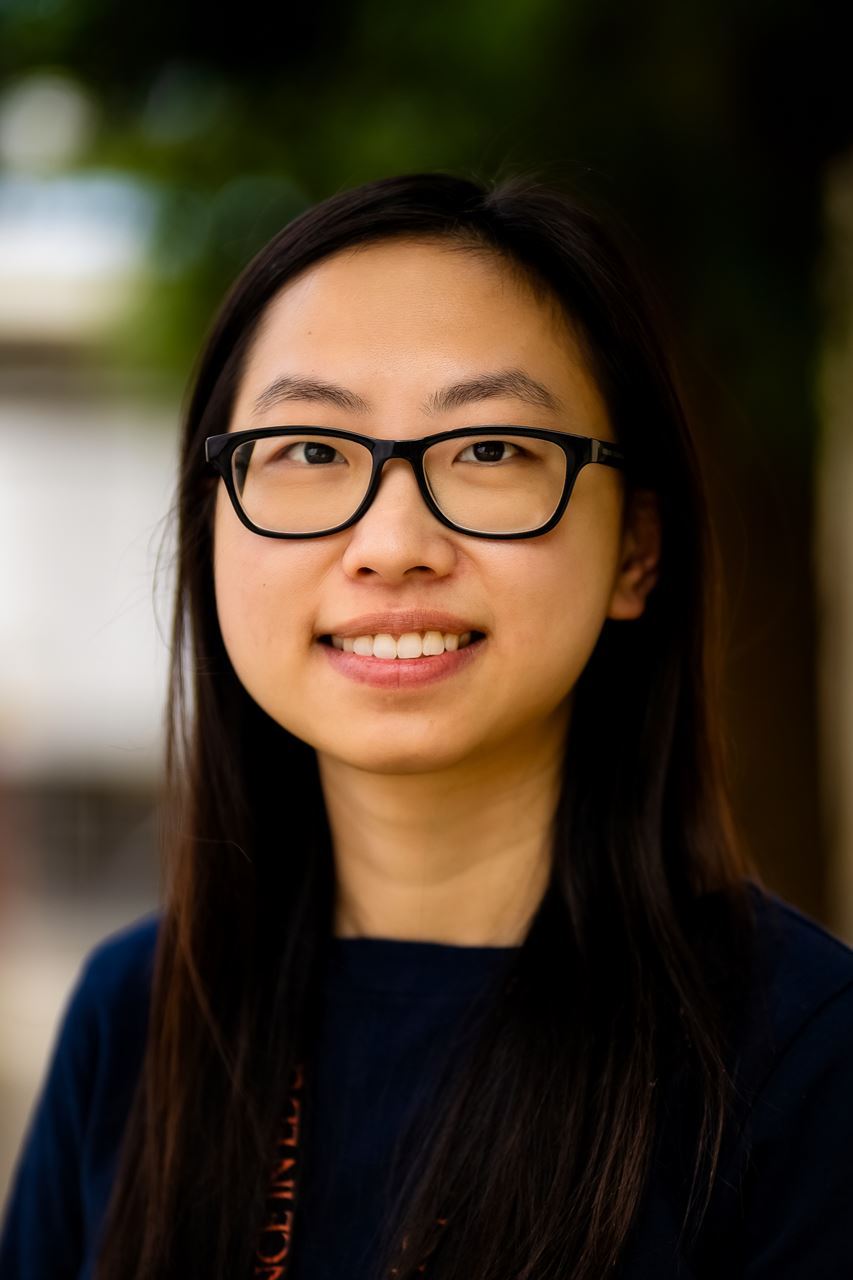
Clinical Pharmacist - Infectious Diseases Kern Medical |